Multidrug-Resistant Fungus Spreading Rapidly In Europe: ECDC
Authored by Naveen Athrappully via The Epoch Times (emphasis ours),
A multidrug-resistant fungus is spreading quickly across hospitals in Europe, posing a major threat to health care systems and patients, the European Centre for Disease Prevention and Control (ECDC) said in a Sept. 11 statement.
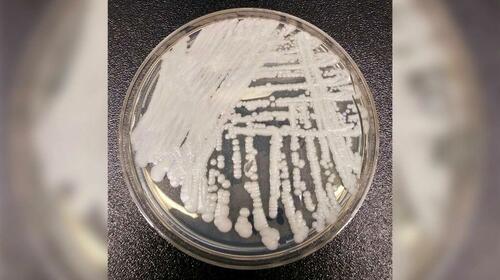
“Candidozyma auris (C. auris) is a fungus that usually spreads within healthcare facilities, is often resistant to antifungal drugs, and can cause severe infections in seriously ill patients. Its ability to persist on different surfaces and medical equipment and to spread between patients makes it particularly challenging to control,” the ECDC said.
“Case numbers are rising, outbreaks are growing in scale, and several countries report ongoing local transmission.”
Symptoms of C. auris infection include fever, high heart rate, low body temperature, fatigue, pain or pressure in the ear, and low blood pressure, according to the Cleveland Clinic.
According to a survey report released by ECDC on Sept. 11, there have been 4,012 cases of C. auris infections or colonization in the European Union (EU) or European Economic Area (EEA) countries between 2013 and 2023. Colonization involves the presence of fungus in a host without causing an illness.
The ECDC says a rapid spread of the infection is due to it becoming endemic in areas where there was no presence earlier.
The top five European nations with the highest C. auris case numbers during this period were Spain with 1,807 incidents, Greece with 852, Italy with 712, Romania with 404, and Germany with 120 cases, according to the report.
Since 2020, case numbers have been increasing rapidly, with 1,346 cases reported by 18 countries in 2023, it said.
“Despite this increase, the recorded case numbers only reflect the tip of the iceberg as systematic surveillance is not in place in many countries,” the report warned.
In Greece, Spain, and Italy, the time period between the first documented C. auris incident and the infection becoming endemic in the region has been five to seven years, “showing how rapidly C. auris can spread through hospital networks.”
“This rapid dissemination of C. auris is of serious concern and points to a high risk for continued C. auris spread throughout European healthcare systems,” the report states. “With increasing C. auris cases and its widespread geographic distribution, sustained control will become more difficult.”
The report suggested implementing early detection and surveillance systems, as well as rapid infection prevention and control measures, to mitigate the impact on patients.
In its statement, ECDC said only 17 out of the 36 EU/EEA nations currently have a national surveillance system to monitor C. auris, with only 15 having developed specific infection prevention and control guidance at the national level.
“C. auris has spread within only a few years—from isolated cases to becoming widespread in some countries,” Dr Diamantis Plachouras, head of ECDC’s Antimicrobial Resistance and Healthcare-Associated Infections Section, said.
“This shows how rapidly it can establish itself in hospitals. But this is not inevitable. Early detection and rapid, coordinated infection control can still prevent further transmission.”
Patients infected or colonized with C. auris can spread the fungus onto objects in health care settings, such as bedrails and doorknobs, according to an April 2024 post by the U.S. Centers for Disease Control and Prevention.
Other individuals may then come into contact with these surfaces, thereby becoming colonized or infected by the fungus, the CDC said.
“C. auris mostly affects patients with severe underlying medical conditions and those requiring complex medical care and invasive medical devices. Invasive medical devices are often necessary but create pathways for C. auris to get into the body,” the CDC said.
Examples of invasive medical equipment include breathing tubes, urinary catheters, and feeding tubes.
“People who do not have these risk factors generally do not carry C. auris or become sick from C. auris. This includes healthcare providers and visitors,” the agency said.
Since 2016, when the first C. auris infection was reported in the United States, the number of clinical cases has continued to rise, according to the CDC. In 2023, there were 4,514 new clinical C. auris cases in the country.
Between 2016 and 2023, there have been a total of 10,788 clinical cases, with California, Nevada, Florida, New York, and Illinois seeing the highest number of incidents.
“However, since 2022 the year-to-year increase has lessened compared to previous years,” the CDC said.
Tyler Durden
Mon, 09/15/2025 – 03:30ZeroHedge NewsRead More


 R1
R1
 T1
T1


